What to Expect When Expecting
Every birth experience is different. This section offers guidance on what may happen during labor and delivery, what recovery can look like, and how to care for your body and mind after birth. The goal is to help you feel prepared to make the choices that are right for you.
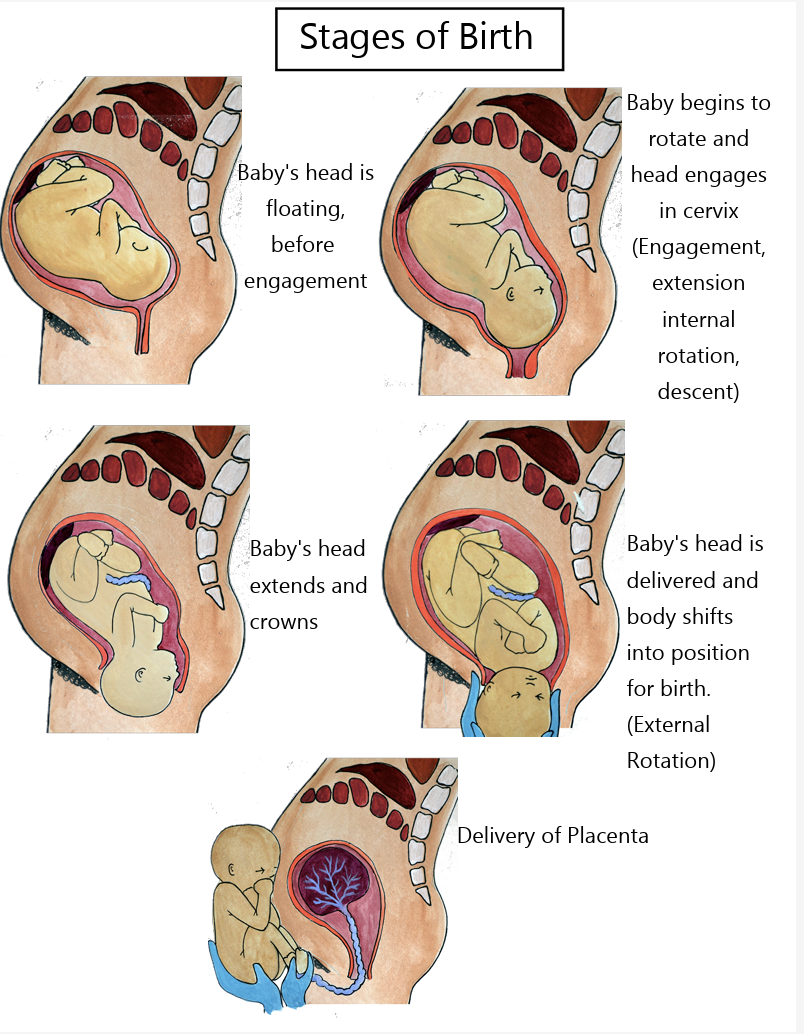
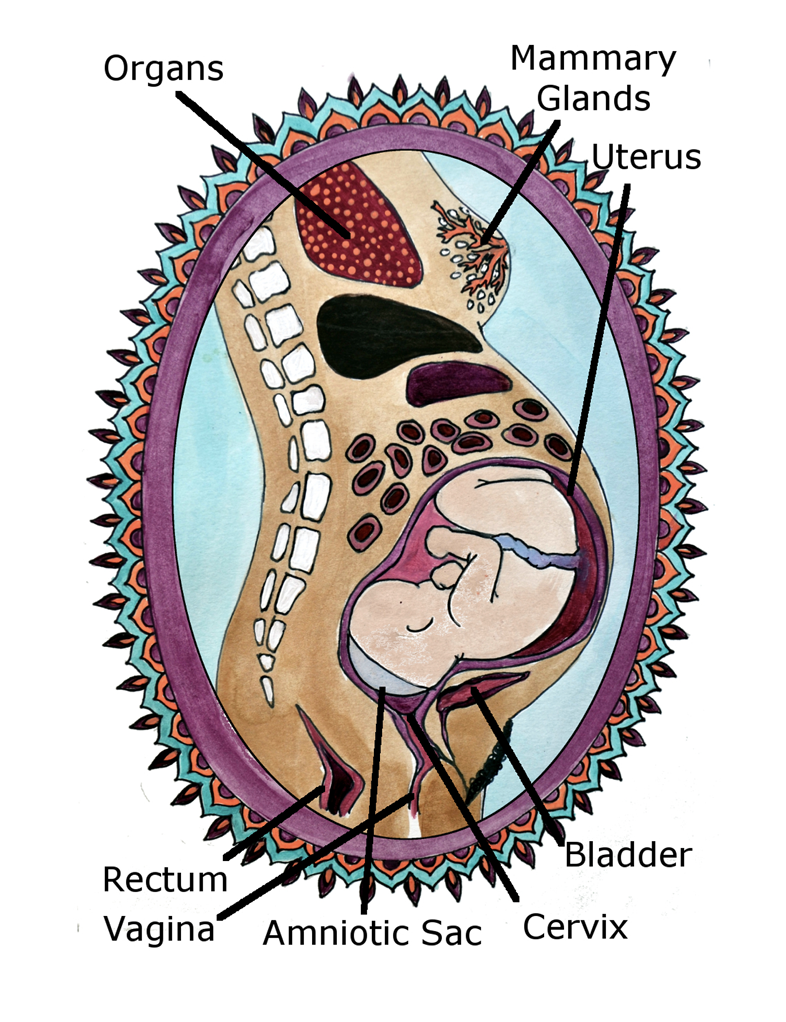
Birthing Process
The birthing process can involve a range of experiences, from early labor through delivery and immediate recovery. This section explains the stages of labor, pain management options, and what to expect in different birth settings.
-
Download any free contraction timer App.
Install baby car seat.
Make "pad-cicles"for after birth perineum care. Pour witch hazel or sitz bath herbs and lavender essential oil onto 8 pads and freeze.
Prepare nourishing food in advance for labor and postpartum. Good labor snacks are fruit, cheese, tea, honey, coconut water, peanut butter, power bars
How to prepare your bed
1. Clean fitted sheet and flat sheet.
2. Plastic mattress cover or tarp included in birth kit.
3. Clean fitted sheet and top sheet. These top sheets you will birth on and after delivery the top sheets are removed and the clean sheets below.
-
Regular mild contractions every 20-30 minutes
Contractions more than 5 minutes apart
Loose mucus plug or have bloody show
Rupture of membranes "waters"
Back pain
Diarrhea or loose stools
-
Download any free contraction timer App. Press start at the beginning of the contraction and stop at the end of the contraction. The frequency of each contraction is from the beginning of one contraction to the beginning of the next. The length of each contraction is from the beginning of one contraction to the end of it. Call and email us a copy of your contraction pattern.
-
It is not unusual for a labor to take 24-36 hours or more. Everyone's experience is different. Listen to your body and your baby.
-
This is the longest part of labor (0cm- 5cm) usually around 12-24 hours for first babies and 2-24 hours for subsequent labors. This stage may stop and start over several days (or typically nights). You will notice contractions or surges that become increasingly consistent and more intense. They may come every 5-10 minutes, sometimes more often, sometimes less.
Common to see increase in vaginal discharge including blood tinged or brownish mucus.
Continue to eat, rest and sleep at regular times.
Do not call friends and family to announce you are in labor.
Call immediately if your waters have released.
-
This is when your midwives will join you! It usually takes around 4-12 hours with first time babies and 2-5 hours for subsequent labors to get from 5 cm to 10cm dilation.
Characterized by contractions getting longer, stronger and closer together.
Contractions every 3-5 minutes, lasting 1 minute for 1 hour.
Common to see more bloody show and spontaneous release of your waters.
Tune inwards as a loving, warm. uninhibited atmosphere will best facilitate this process.
Empty your bladder frequently and change positions often, eat and drink as desired.
-
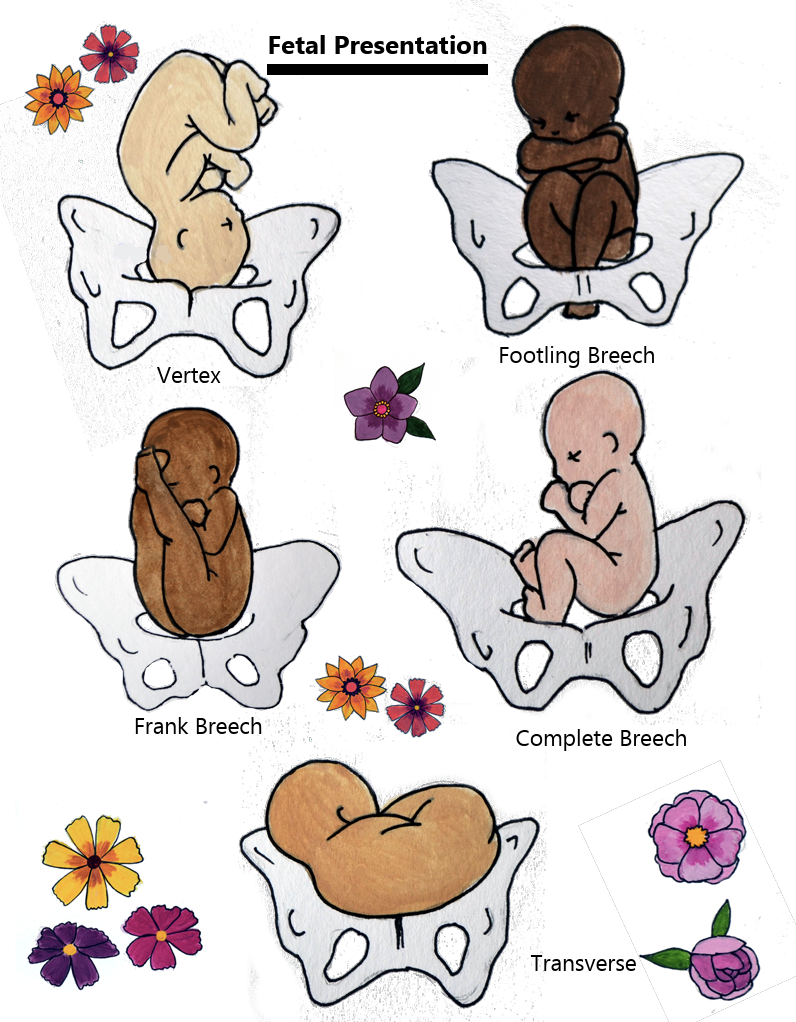
Before the urge to push comes there may be a natural lull or rest phase. This may last a few minutes to a few hours. This is known as "rest and be thankful". The urge to push is a strong reflex that you will not be able to ignore. Listening to your natural urges will allow your body to gently stretch and birth your baby. We will offer positions to optimize your pelvic shape which can reduce length of labor and tears. Some positions are squatting, hands and knees, sitting on the toilet, lying on your side. It is always best to follow your instincts. We will be listening to your baby frequently and assessing both your vitals.
-
Your Midwives will help to receive your baby, or you or your partner may help catch your baby. Immediately after birth we will bring your baby to your chest or abdomen for warmth and skin to skin contact. Some babies need some support during the first few minutes as they transition to life outside your body for this reason we practice delayed cord cutting. Talk to your baby, breathe deeply and send your baby love! Allow yourself to be totally absorbed in your new baby, gazing, touching and talking to them. Your baby may look to nurse after a few minutes. Let them find your nipple as this journey is important. We will closely monitor you and your baby and watch for signs that your placenta is releasing. The placenta usually comes on it's own in the first 15-30 minutes. We may get you into another position to help facilitate this. We delay cutting the cord and will catch it in a bowl and then give you the option to see the incredible organ that grew and housed your baby! We will help facilitate nursing, assess everyone's vitals, perform a newborn exam (which includes weighing and measuring baby), check for tears and place stitches if necessary. You can breastfeed right away for as long as you and your baby desire. Your baby should remain on your body for warmth and comfort. This is a magical time of bonding!
Postpartum Journey
The postpartum journey includes physical healing, emotional changes, and adjusting to life after birth. This section provides information on recovery, newborn care, and feeding.
-
You must register the birth with the Department of Vital Statistics within 10 days of the birth, however you have up a one year. There is no fee within the first year and you must bring your baby, all necessary paperwork, photo IDs and both parents to the appointment. If both parents can not go, they can go at separate times or both do not have to be on it.
Department of vital statistics Call to make an appointment (213) 288-7812
-
First few days expect heavy period like bleeding. Bleeding should be bright red with some small clots. Bleeding can last from 10 days to 4 weeks, gradually getting lighter to spotting and mucus.
During the first three days empty your bladder every 2 hours while awake.
Check your bleeding and make sure your uterus is firm after you pee.
If your uterus isn't firm or you are bleeding more frequently, put baby to breast and rub your uterus until it is a firm ball.
Express a little colostrum or breastmilk and rub it into nipples after each feed. This will help the skin stay lubricated and reduce nipple soreness. Milk will come in around 48-72 hours. If you get uncomfortably engorged, nurse more often and use a warm compress on your breasts / chest.
The more rest and laying in during the first two weeks post partum the quicker your pelvic floor will heal.
Start Kegel exercises immediately, especially when standing!
Do not use ice packs 24 hours after birth.
Sleep when your baby sleeps! Read more
Eat and drink regularly. Get lots of protein, vitamin C, iron, calcium, and fiber. This will help with milk production and overall recovery.
CONTACT IMMEDIATELY:
Fever above 99.5
Bleeding more than 1 saturated pad an hour
Blood clots bigger than an egg
Belly pain or foul smelling discharge
Pain with urination
Painful, warm, red lump in breast
-
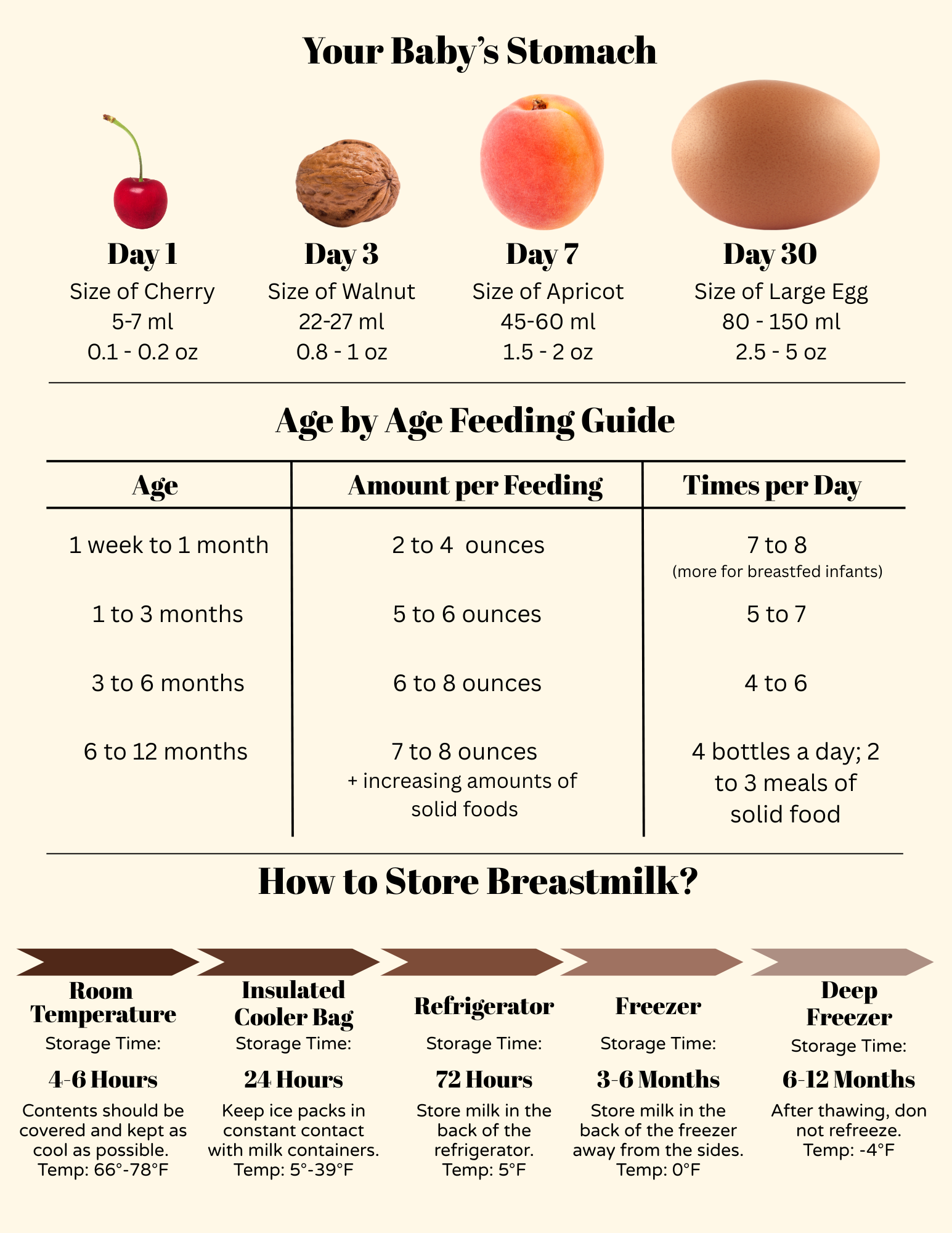
First milk is called "colostrum" it is thick yellow liquid is loaded with protein & antibodies.
Nurse whenever your baby shows an interest. Signs of this are rooting, licking hands, lip smacking.
Nurse every 2-3 hours during the day & every 3-4 hours at night. If baby goes longer it is important to wake them up to feed.
Check baby's diaper for meconium and urine regularly. This will ensure that baby is getting enough to eat and that their systems are working.
Expect to see pee equal to the number of days of life. For example, by day three baby should have at least three pees.
Observe baby's color, temperature and breathing. Observe the cord for odor, drainage and redness.
Newborn normal temperature range 97.5-99.5 by armpit.
If your baby is slightly above or below this range then adjust your baby's clothing and the room temperature and recheck in about an hour.
It is normal for a baby to spit up amniotic fluid in the first 24-36 hours after birth.
CONTACT IMMEDIATELY:
Fever above 99.5 armpit
Grunting, nose flaring or respiratory rate over 60 breaths minute
Jaundice or generalized blue or grey color
No urination or bowel movement in the first 24 hour
Blue color around the mouth or trunk of body
-
When in doubt just put them to breast/chest! Nurse on demand as frequently as your baby wants, for as long as they want. Face baby's belly to your belly & aim their nose to your nipple. Experiment with different positions; laid back, side lying and football hold.
-
Your baby should eat double their weight in ounces per day.
Ensure a good latch by making sure baby's mouth is covering your entire areola.
It is normal for babies to lose around 10% from their birth weight in the first two weeks.
They need 2-3 ounces per feeding.
-
While studies on the benefits and effectiveness of placenta eating are lacking, there are many anecdotal reports that it helps support a happier and smooth postpartum transition. Placenta consumption may lead to many advantages such as better mood, increased energy, increased milk production, lower chances of anemia and lower chances of the 'baby blues' or postpartum depression. There are 3 main hormones contained in the placenta:
1. Oxytocin: helps bonding, pain relief, and helps with milk production and supply.
2- HPL (Human Placenta Lactogen): promotes the production of prolactin which allows milk production.
3- POEF (Placenta Opioid Enhancing Factor): Pain reliever.
Traditional Chinese method
For thousands of years, Traditional Chinese Medicine "TCM" has recognized the placenta as powerful medicine. It is used to augment the "Qi" also known as "life force energy", nourish the blood, and augment the kidney essence. This school of thought suggests that the dried placenta is used to bring the postpartum body back into balance, replenishing what was lost during childbirth. The traditional process of TCM placental preparation involves lightly steaming the placenta with organic lemon and cayenne which is believed to form the action of the placenta medicine. In this process the placenta is steamed with these herbs, sliced thin and dehydrated. It is then ground into a powder and put into capsules. Adding heat to the placenta is part of what makes TCM style encapsulation unique. In Chinese medicine raw foods are generally considered "cooling" and to be avoided in the postpartum period. Within the TCM framework, raw placenta is considered cooling and isn't recommended in the postpartum as a general rule for the tonifying purposes of nourishing blood and restoring energy.
The raw method
If you desire to consume your placenta, we recommend the way mammals do after birth by ingesting it raw. This way, no nutrients are degraded or lost and hormones are not affected. This method skips the steaming step and the placenta is dehydrated, ground, and then the capsules are filled. There is less research to support this preparation but it has become the most widely performed preparation of placenta medicine. The raw method is thought to retain much of the hormones and nutrients. However, we do not know the effect of steaming/cooking. This method generally yields more capsules as there is some shrinkage during steaming with the traditional method. Other options for ingestion include raw smoothies and tinctures. Raw smoothies are the best way to take your placenta ‘raw’, even over the raw encapsulation method. Here, small pieces of frozen placenta can be blended with fruit and juice/liquid to create a smoothie in which the taste of the placenta is undetectable. We recommend making these recipes in advance and store in your freezer.
Raw recipes
Tropical fruit: 1 cup coconut milk, 1/2 cup pineapple, 1/2 cup mango, 1/4 cup frozen berries, 1/3 cup spinach, Juice from one lime, 1 tbsp flax seed meal for Omega-3’s, 1 tbsp dry quinoa whole or ground for protein, 1 cubic inch of placenta, about the size of a strawberry
Fruit & veggie: 4 frozen strawberries, 1/3 cup frozen blueberries, 1 banana, 4 baby carrots, 1/3 cup spinach, 3/4 – 1 cup cran-grape juice or any flavor juice, 1 tbsp flax seed meal for Omega-3’s, Dollop of honey, 3 ice cubes, 1 cubic inch of placenta, about the size of a strawberry
Vanilla yogurt: 1 cup yogurt (Greek yogurt preferred), 1 banana, 3 frozen strawberries, 1 tsp vanilla, 1 tbsp flax seed meal for Omega-3’s, 1 tbsp dry quinoa whole or ground, Dollop of honey 1 cubic inch of placenta, about the size of a strawberry
How long is the process?
Encapsulation is a two day process and picked up the day of birth. On day 1 the placenta is prepared for dehydration and the drying process is started. On day 2 the dried placenta is ground and transferred into capsules.
When should I not encapsulate?
If it is not kept chilled, bacteria may grow and consumption should be avoided. If you developed an infection during labor, immediate postpartum, received Pitocin, antibiotics or an epidural during labor you should not consume your placenta.
Can I encapsulate from a previous birth?
It is best if the encapsulation is done within 48 hours of the birth, however, a previously frozen placenta can be encapsulated. The general guideline is that the frozen placenta should not be much more than 6 months old. If your placenta is older than this you may chose to explore other options like burial. Placenta prints are not possible with a frozen placenta due to the consistency of the blood after thawing.
How many will I get and how long will they last?
The number of pills varies between 25-200 depending on the size of the placenta. Around 50 "00" pills is common. Depending on the quantity of pills, you can take them up to 4-6+ weeks postpartum. If you choose to stop taking the pills before then, the pills may be stored in the freezer.
How much should I take?
Take 2 capsules 3 times a day for the first two weeks and then slowly reducing the dose until you no longer need them. Begin taking them on day 3-4 after your milk comes in.
How do I get my placenta from the hospital?
It's your right to keep your placenta after birth. You will need to find out the requirements and paperwork needed from your hospital. Encapsulation is not recommended for cesarean births, as you will have received medications that are contraindicated for consumption, but you may keep it for ceremonial purposes. The hospital will not release your placenta if you have an active infection or chorioamnionitis. If your placenta is sent to pathology it will come into contact with chemicals that should not be consumed.
Labor and Birth
A Visual Guide
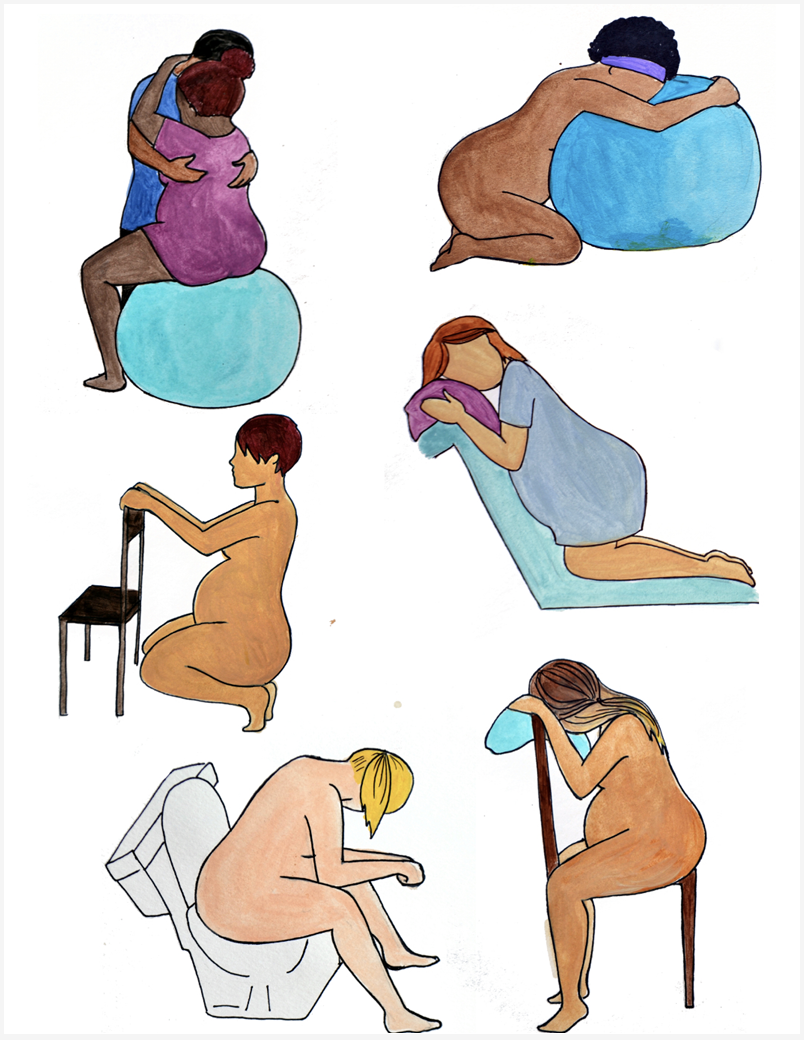
Birthing Positions
Birthing positions can influence comfort, labor progress, and how supported you feel during birth. Here are some examples of the many birthing positions.
Fertility in the Postpartum
After childbirth, your body begins to change in ways that can affect fertility and ovulation. This section provides information to help you understand when fertility may return, how it varies from person to person, and the options available to support your reproductive goals—whether that means spacing pregnancies or trying to conceive again.
When it Returns
Timing of ovulation varies for each person. Earliest ovulation can occur 30-35 days after birth and up to 12 months. The average period returns at 14.6 months.
Timing of ovulation varies due to the length of suckling & time intervals between feedings. Likely to occur when down to only two feedings at night.
When period returns, ovulation occurred 14 days before. First spotting can be a sign of ovulation.
Rare to get pregnant with first ovulation but can happen!
It is possible to have one or more periods before you start ovulating.
Cyclical cramping or PMS-type symptoms for weeks or months before period begins could be a sign of fertility returning.
How to Delay
Nursing on cue stimulates prolactin which provides suppresses ovulation.
Nursing no longer than 4 hrs during the day and 6 hrs at night between feedings.
Keep baby close both day and night and allow comfort feedings for baby.
Do not use bottles or pacifiers.
Exclusive breastfeeding by itself is 98-99.5% effective when baby is less than 6 months old.
Rates of pregnancy with this method: first 3 months around 0%, 3-6 months is less than 2%, after 6 months is 6% (assuming menstruation has not returned).
Using Contraception
When babies vary their feeding frequency and occasionally sleep through the night.
If supplementing with formula or with any changes in feeding or frequency in a 24hr period.
When period returns.
If you are unsure about this method, begin using contraception 21 days after birth.
Resume oral contraception on day 21 or contraceptive protection.
Fertility Awareness Method should start after first returned period.
Note 14 days before period for date of ovulation.
Need Additional Support?
Our goal is to help families seeking support during their birthing and postpartum journey. If you are interested in learning more about how we can support you and your family, schedule a consultation.